Case management sits at the heart of many human and social service nonprofits. When it works well, clients experience smoother access to services, less repetition, fewer missed handoffs, and better outcomes. When it’s fragmented, clients can fall through gaps, staff spend more time chasing information than supporting people, and reporting becomes a scramble.
This guide breaks down case management models in plain language, with nonprofit realities in mind: limited resources, complex client needs, multi-partner ecosystems, and high expectations for accountability.
You’ll learn the five most common models of case management, what each is best for, and how to decide which approach fits your mission, staffing, and community context.
We’ll also walk through practical implementation tips and the role technology can play—where a purpose-built platform like Sumac nonprofit case management software can support case management consistency and outcomes without adding administrative burden.
What “Case Management Model” Means in Practice
A case management model is essentially your organization’s operating philosophy for coordinating support around a client. It defines:
- How clients enter services: referrals, outreach, walk-in, screening
- How needs are assessed: standard tools, clinical assessments, strengths-based methods
- How plans are created and updated: who leads, how often, client involvement
- How services are delivered: direct service vs. referral-driven, in-house vs. partners
- How progress is tracked: touchpoints, milestones, outcomes, documentation
- How decisions are made: case conferencing, clinical supervision, triage rules
Importantly, many nonprofits don’t use a single pure model – they use a hybrid. The goal isn’t academic perfection; it’s building a coherent approach staff can follow and clients can understand.
For a strong grounding in standard functions and principles of case management, the Case Management Society of America (CMSA) provides a widely cited overview of case management practice and roles.
The “5 Models of Case Management” Nonprofits Encounter Most Often
When people search for the 5 models of case management, they’re usually looking for the core approaches most widely used across human services. Here are five that show up repeatedly in nonprofit practice, plus where each tends to fit best.
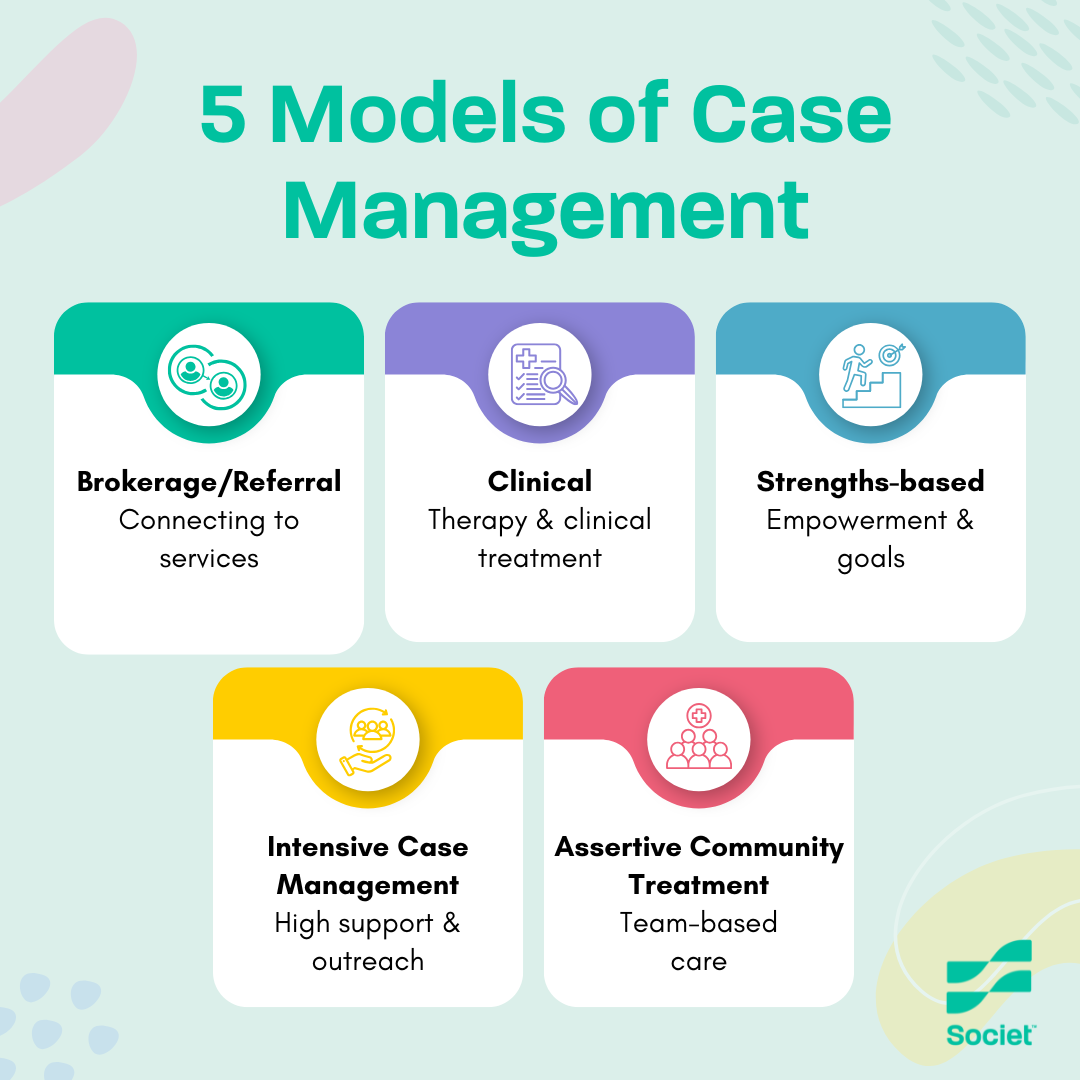
1) Broker (or Referral) Model
What it is: The case manager primarily assesses needs, connects clients to services, and coordinates referrals, but does not provide most services directly.
Best for:
- Organizations with limited direct-service capacity
- Communities with strong partner networks
- Short-term interventions where navigation is the main barrier
Watch-outs:
- Clients can experience “referral fatigue” if partners aren’t coordinated
- Outcomes depend heavily on external service availability
- Requires excellent relationship management with community provider
What good looks like: Clear referral pathways, warm handoffs, follow-up loops, and documentation that tracks whether the referral actually turned into service.
Sumac makes this easy by centralizing referrals, follow-ups, and outcomes so staff can see—at a glance—what’s been completed and what still needs action.
2) Clinical (or Therapeutic) Model
What it is: Case management is integrated with clinical assessment and intervention. The case manager often has clinical training and may deliver therapy-informed supports, behavioral health coordination, and structured treatment planning.
Best for:
- Mental health and addictions programs
- Complex trauma contexts
- High-risk populations requiring clinical oversight
Watch-outs:
- Risk of “over-clinicalizing” non-clinical needs (housing, income, food)
- Requires supervision structures, clinical governance, and documentation rigor
- Can be staff-intensive
What good looks like: Integrated care plans, clear consent protocols, standardized assessments, and strong collaboration with medical/behavioral health partners.
Sumac makes this easy by supporting configurable assessments, secure documentation, and shared care plans that align clinical rigor with day-to-day workflows.
3) Strengths-Based Model
What it is: Focus shifts from deficits to capabilities, goals, and assets. The case manager partners with the client to identify strengths and build a plan that emphasizes empowerment and self-determination.
Best for:
- Youth services
- Family support
- Employment readiness and community reintegration
- Programs aiming to reduce dependence on systems
Watch-outs:
- Must still address urgent risks and structural barriers directly
- Requires staff training to avoid “toxic positivity” (ignoring real hardship)
What good looks like: Client-led goal setting, motivational interviewing techniques, and progress tracking that includes both outcomes and capacity-building steps.
Sumac makes this easy by allowing organizations to track goals, milestones, and strengths alongside services—so progress reflects the whole person, not just program outputs.
4) Intensive Case Management (ICM) Model
What it is: Lower caseloads, frequent contact, proactive outreach, and hands-on support. The case manager may accompany clients to appointments, coordinate across multiple systems, and deliver sustained follow-up.
Best for:
- People experiencing chronic homelessness
- Justice-involved clients
- Individuals with multiple co-occurring challenges
- Situations where missed appointments or fragmented care is common
Watch-outs:
- Resource heavy (time, staffing, travel)
- High risk of staff burnout without boundaries and support
- Needs clear criteria for “step-down” and transitions
What good looks like: Defined intensity levels, escalation protocols, caseload caps, team coverage, and outcome metrics that reflect stability over time (not just quick wins).
Sumac makes this easy by giving case managers clear visibility into caseloads, contact frequency, and longitudinal outcomes—without adding administrative overload.
5) Assertive Community Treatment (ACT) / Team-Based Model
What it is: A multidisciplinary team (not just one case manager) delivers coordinated, community-based support—often for individuals with severe mental illness or high acuity needs. Services are brought to the client, not the other way around.
Best for:
- High-acuity behavioral health populations
- Programs needing 24/7 coverage or rapid response
- Communities with established ACT standards and clinical staffing
Watch-outs:
- Complex to implement and govern
- Requires staffing mix (clinical, psychiatric, peer, employment, etc.)
- Needs shared documentation systems and team routines
What good looks like: Daily/weekly team huddles, shared caseload ownership, consistent care planning, and strong data visibility across the team.
Sumac makes this easy by enabling shared records, role-based access, and real-time collaboration so multidisciplinary teams stay aligned around the same client story.
Other Common Models of Case Management (Beyond the “Top 5”)
Depending on your sector, you may also run into:
- Transitional case management: Time-limited support during a major transition (hospital discharge, shelter-to-housing, foster care aging out).
- Wraparound model: Often used in children/youth and family systems; integrates formal wraparound services and natural supports (family, community) into one plan.
- Critical Time Intervention (CTI): A structured, time-limited approach that emphasizes transitions and building durable community supports.
- Peer-led case management: Peers with lived experience provide navigation and engagement, often improving trust and retention.
According to NASW Standards for Social Work Case Management, these can be standalone or layered onto the five core models above.
How to Choose the Right Model (A Decision Framework)
Most nonprofits don’t fail because they picked the “wrong” model—they struggle because the model doesn’t match constraints, referral ecosystems, or client acuity. Use these questions to align strategy with reality:
1) What’s the primary barrier for your clients?
- Access/navigation barrier: Broker model may fit
- Behavioral health complexity: Clinical or ACT may fit
- System fragmentation + high need: ICM may fit
- Low trust/engagement: Strengths-based and peer components may fit
2) What does your staffing and supervision structure support?
A clinical model without clinical supervision is risky. ACT without multidisciplinary staffing becomes “ACT in name only.” Be honest about the infrastructure you can sustain.
3) What does your community service landscape look like?
If partner capacity is limited (long waitlists, few providers), a broker model can unintentionally become a “dead end.” You may need more direct service or more intensive support.
4) How will you measure success?
Choose metrics that match the model:
- Broker: referral completion rates, time-to-service, retention
- Strengths-based: goal attainment scaling, skill-building milestones
- ICM/ACT: stability measures, reduced crisis episodes, sustained housing or engagement
- Clinical: symptom/function measures, treatment adherence, improved wellbeing
Implementation: The Difference Between “We Do Case Management” and “We Deliver Outcomes”
Even excellent models can collapse without operational clarity. The nonprofits that perform best tend to standardize these five areas:
- Intake and eligibility rules
Clear triage criteria prevent caseload overload and help clients understand expectations. Social work case management software, like Sumac, can help streamline and triage intake. - Assessment and care planning templates
Consistent tools reduce variability and protect quality when staff turnover happens. - Contact cadence and service standards
Define what “active” means (e.g., minimum touchpoints, outreach attempts, follow-up rules). - Documentation workflows that match reality
If documentation is too heavy, it won’t happen. If it’s too light, reporting and continuity suffer. - Continuous improvement loops
Use case reviews, supervision, and dashboards to spot patterns (drop-off points, bottlenecks, inequities).
Where Technology Helps (Without Turning Staff Into Data Clerks)
Case management models live or die on coordination, consistency, and visibility. That’s where software can quietly make a big difference—especially when it’s designed specifically for human and social service nonprofits.
A platform like Sumac can support your model by helping you:
- Centralize client records and reduce duplicate data entry
- Standardize assessments and care plans with configurable templates
- Track referrals, follow-ups, and outcomes in one place
- Support team-based collaboration (notes, tasks, permissions)
- Produce funder-ready reporting without manual spreadsheet wrangling
The key is alignment: the software should reinforce your chosen models of case management, not force staff into a workflow that doesn’t match how your services are delivered.
A simple litmus test: if staff say, “This system makes it easier to serve clients,” you’re on the right track. If they say, “This is for reporting, not for us,” the tool isn’t supporting your model.
A Practical Way to Move Forward: Start With a Model “Definition Sprint”
If your organization is unsure which approach you’re using—or you suspect every staff member is doing it differently—run a short, structured sprint:
- Map your current client journey (referral → intake → assessment → plan → services → exit)
- Identify your real constraints (caseload, staffing, partner capacity)
- Choose your default model (and where you’ll use hybrid elements)
- Define service standards (touchpoints, documentation, escalation, step-down)
- Configure templates and reporting (ideally inside your case management software)
- Train and reinforce with supervision, not just a one-time workshop
This is often the fastest path to better outcomes—because it turns “tribal knowledge” into a shared operating system.
Final Thought: The Best Case Management Model Is the One Your Team Can Deliver Consistently
Nonprofits don’t need the most sophisticated model—they need the most fit-for-purpose model. Start with client needs and operational reality, build a clear standard of practice, and support it with tools that reduce friction.
If your organization is refining its approach and wants software that can adapt to how human and social services actually work, Sumac is worth a look as a case management platform designed to support nonprofit workflows—especially when consistency, outcomes, and funder reporting all matter at once.